+86-18343147735
+86-18343147735




In recent years, the field of In Vitro Diagnostic (IVD) testing has experienced transformative advancements. A report from the International Diagnostic Industry Association notes a projected growth of the IVD market, reaching over $100 billion by 2026. This growth can greatly enhance patient outcomes, yet challenges remain in optimizing these tests.
Dr. Emily Chen, a leading expert in IVD technology, states, “Effective optimization is crucial for increasing the accuracy and efficiency of diagnostic tests.” This highlights the need for continuous improvement in testing processes. Issues such as standardization and integration into clinical workflows must be addressed. Moreover, despite rapid technological progress, disparities in access to advanced diagnostic tools persist.
Achieving better patient outcomes in IVD requires a multi-faceted approach. Collaboration among industry stakeholders, healthcare providers, and regulatory bodies is essential. A focus on education and training for personnel is also vital. As the IVD landscape evolves, stakeholders must reflect on existing practices to ensure they are not only effective but equitable.

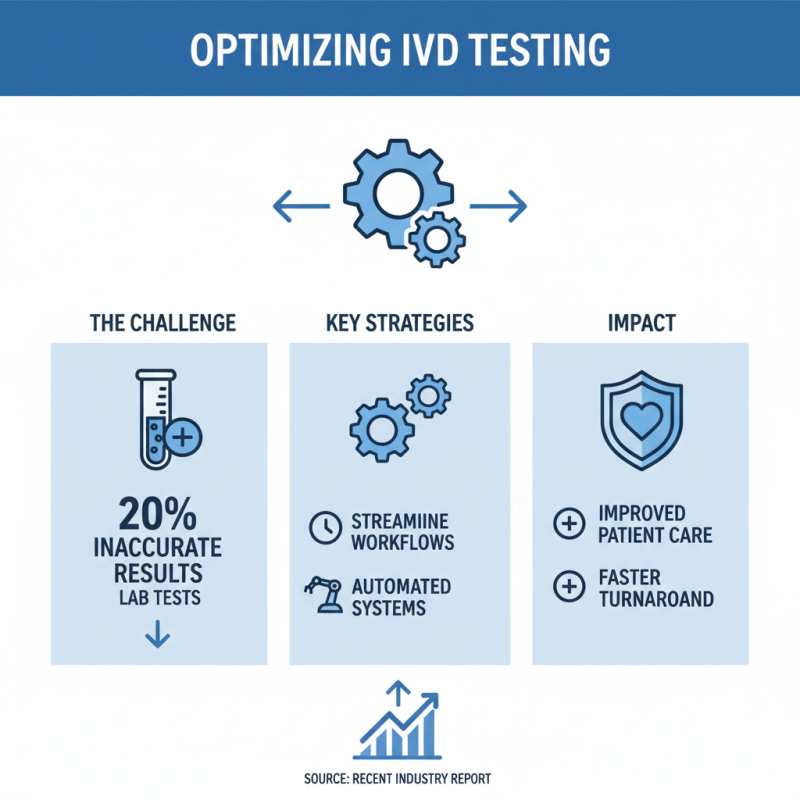
In vitro diagnostic (IVD) testing is crucial for patient care, but optimizing its efficiency remains a challenge. According to a recent report, nearly 20% of lab tests yield inaccurate results. This highlights the need for improved testing strategies. Streamlining workflows can reduce turnaround times. Implementing automated systems might enhance accuracy and efficiency.
Collaboration between laboratories and clinicians can bridge gaps in communication. Regular feedback on test results can lead to better interpretation and utilization. Data suggests that better integration of patient histories can improve testing relevance. As we move towards precision medicine, personalized testing could yield better patient outcomes. However, it can be resource-intensive.
Despite advancements, many labs still rely on outdated processes. This can hinder innovation. Training staff on new technologies is essential but often overlooked. Reports indicate that 30% of lab personnel feel inadequately trained. Investing in training can drastically impact patient care and lab efficiency. As the landscape evolves, we must remain vigilant and adaptable to optimize these essential diagnostic tests.
The integration of advanced technologies in diagnostic testing is reshaping patient care. New tools and techniques enhance accuracy and speed. These innovations can lead to earlier detection of diseases. For instance, AI-driven algorithms analyze complex data patterns swiftly. However, the implementation often faces hurdles. Technical expertise is required, which may not be available everywhere.
Moreover, patient data privacy raises ethical concerns. Continuous adaptation to regulatory standards is necessary. Many facilities struggle to keep up with evolving technologies. Despite this, the potential for improved patient outcomes is significant. Real-time monitoring devices provide immediate feedback. This could change how conditions are managed, but challenges remain.
Optimizing these advancements should focus on user-friendly applications. Streamlining processes can alleviate some operational burdens. Collaboration between tech developers and healthcare professionals is crucial. It can bridge gaps in understanding and usability. While progress is evident, there is a long journey ahead. Each step must consider both innovation and patient needs.
Engaging patients in the diagnostic process is crucial for better health outcomes. Many patients feel disconnected and uninformed when it comes to their testing. This can lead to anxiety and mistrust in the healthcare system. Instead, healthcare providers should prioritize clear communication. Offering information that is easy to understand is essential. Patients need to know what tests they are undergoing and why.
Incorporating technology can enhance patient engagement. For example, mobile apps can notify patients of their test results in real-time. However, some patients may struggle to navigate these digital platforms. Training and support could help bridge this gap. The goal is to make patients feel like active participants, not just passive recipients of care.
Moreover, feedback mechanisms should be in place. Patients should have the opportunity to share their experiences. This can guide improvements in the diagnostic process. Yet, we often overlook this step. Addressing patient concerns can lead to a more personalized approach. It is not just about the results, but also about how patients feel throughout the journey.
Establishing robust quality standards for in vitro diagnostics (IVD) is crucial for enhancing patient outcomes. A 2023 report indicated that nearly 70% of clinical decisions are influenced by laboratory results. However, over 40% of diagnostic errors can be traced back to pre-analytic phases, including specimen collection and handling. This highlights the critical need for stringent quality control protocols.
Current regulations vary significantly across regions, leading to disparities in test accuracy. For instance, some reports suggest that unverified IVD products can lead to misdiagnosis rates as high as 25%. This inconsistency in quality not only affects patient trust but also strains healthcare resources. Establishing consistent global standards would mitigate these risks.
Furthermore, training healthcare professionals involved in the IVD process is essential. A WHO study revealed that inadequate training contributes to a staggering 20% of pre-analytic errors. Regular workshops focusing on quality protocols could bridge this gap. The time to reflect on these shortcomings and pursue a cohesive approach to quality in IVD is now. Quality isn’t just about compliance; it directly impacts lives.
In vitro diagnostic (IVD) testing is vital for improving patient outcomes. Analyzing data effectively can enhance decision-making in patient care. According to a recent report by the World Health Organization, better data utilization in healthcare can lead to a 15% increase in diagnostic accuracy. This statistic highlights the necessity for healthcare professionals to harness data-driven insights.
Often, healthcare providers struggle with data interpretation. A 2022 study revealed that over 40% of clinicians feel overwhelmed by the volume of data available to them. This gap poses a challenge. Simplifying data presentation could alleviate this pressure. Visual summaries and dashboards can transform complex data into digestible insights.
Tips for optimizing data analysis include prioritizing data relevance. Focus on information that impacts patient care directly. Engage with clinical decision support tools to streamline patient assessments. Regular team training on data interpretation can enhance overall competency. The goal is to foster a culture of informed decision-making. A reflective approach to data is essential; understanding past missteps can lead to significant improvements. Adopting a mindset of continuous learning will ensure better patient outcomes through optimized IVD testing.